Male Infertility Services
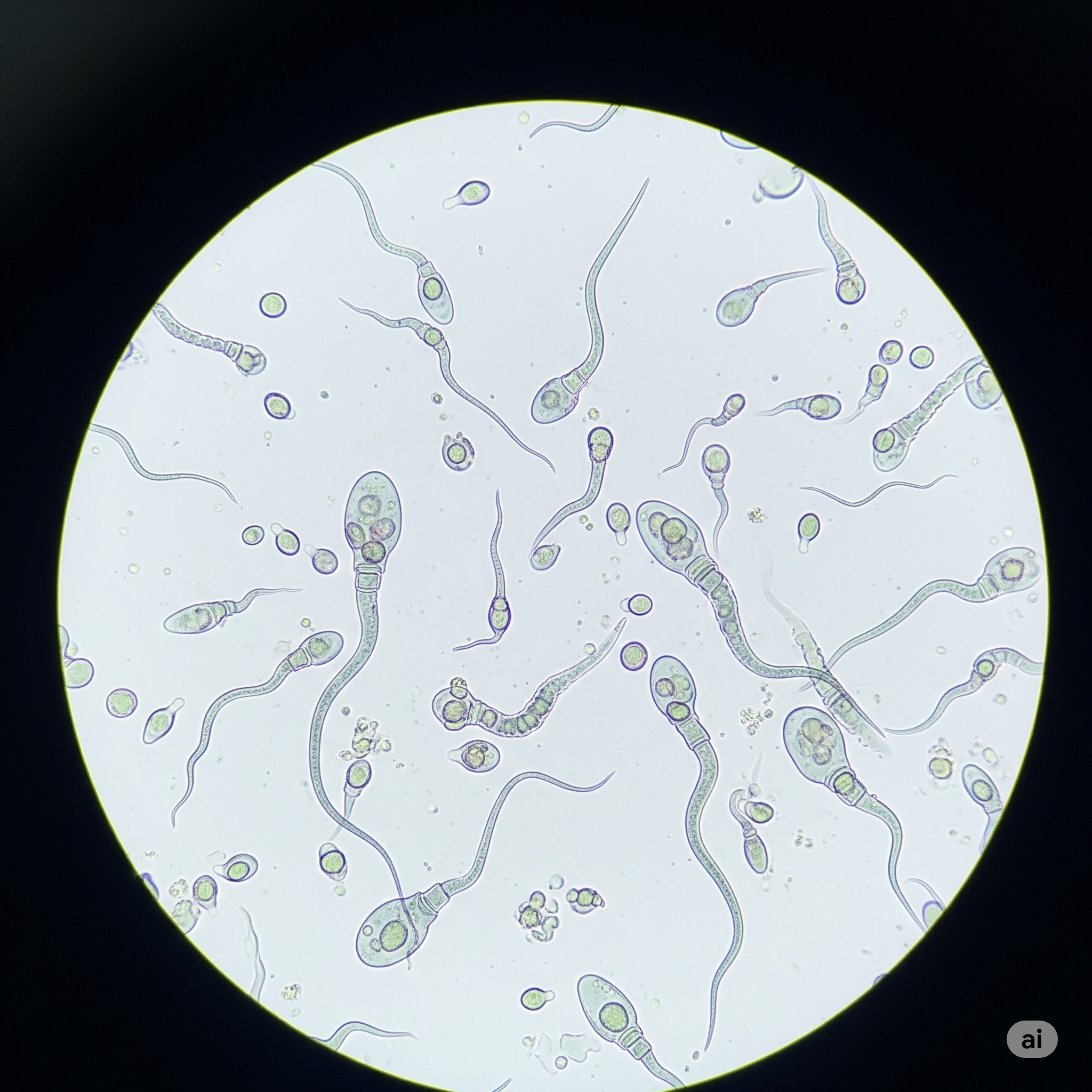
Semen Analysis
Semen analysis is the crucial first step in evaluating male fertility. It assesses key parameters like sperm count, motility (movement), and morphology (shape) to provide vital insights into sperm production and overall ejaculatory health. This test helps identify potential underlying issues and guides subsequent fertility treatments.
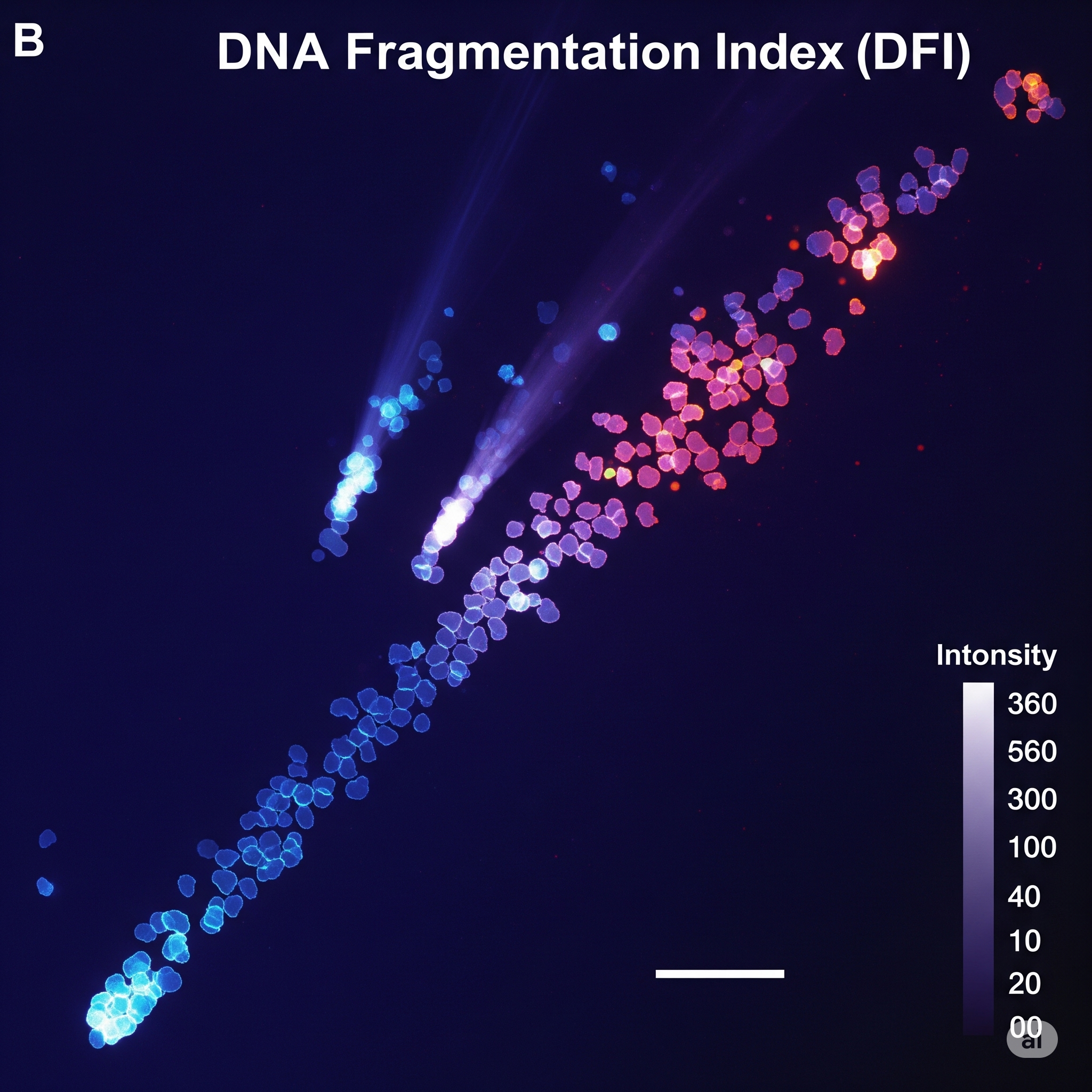
DNA Fragmentation Index (DFI)
The DFI is an advanced diagnostic test that measures the integrity of sperm DNA, revealing the extent of DNA breaks or damage. High levels of DNA fragmentation can contribute to unexplained infertility, recurrent IVF failures, or miscarriages. This assessment offers deeper insights beyond standard semen analysis, helping us tailor effective treatment strategies.
Low Sperm Analysis And Treatment (Oligospermia)
Oligospermia, or low sperm count, is a common male infertility factor. Our clinic provides thorough analysis to pinpoint the causes, which can range from hormonal imbalances to lifestyle factors. We then develop a personalized treatment plan, incorporating medical management, lifestyle changes, or assisted reproductive technologies (ART) to improve sperm concentration and enhance fertility outcomes.
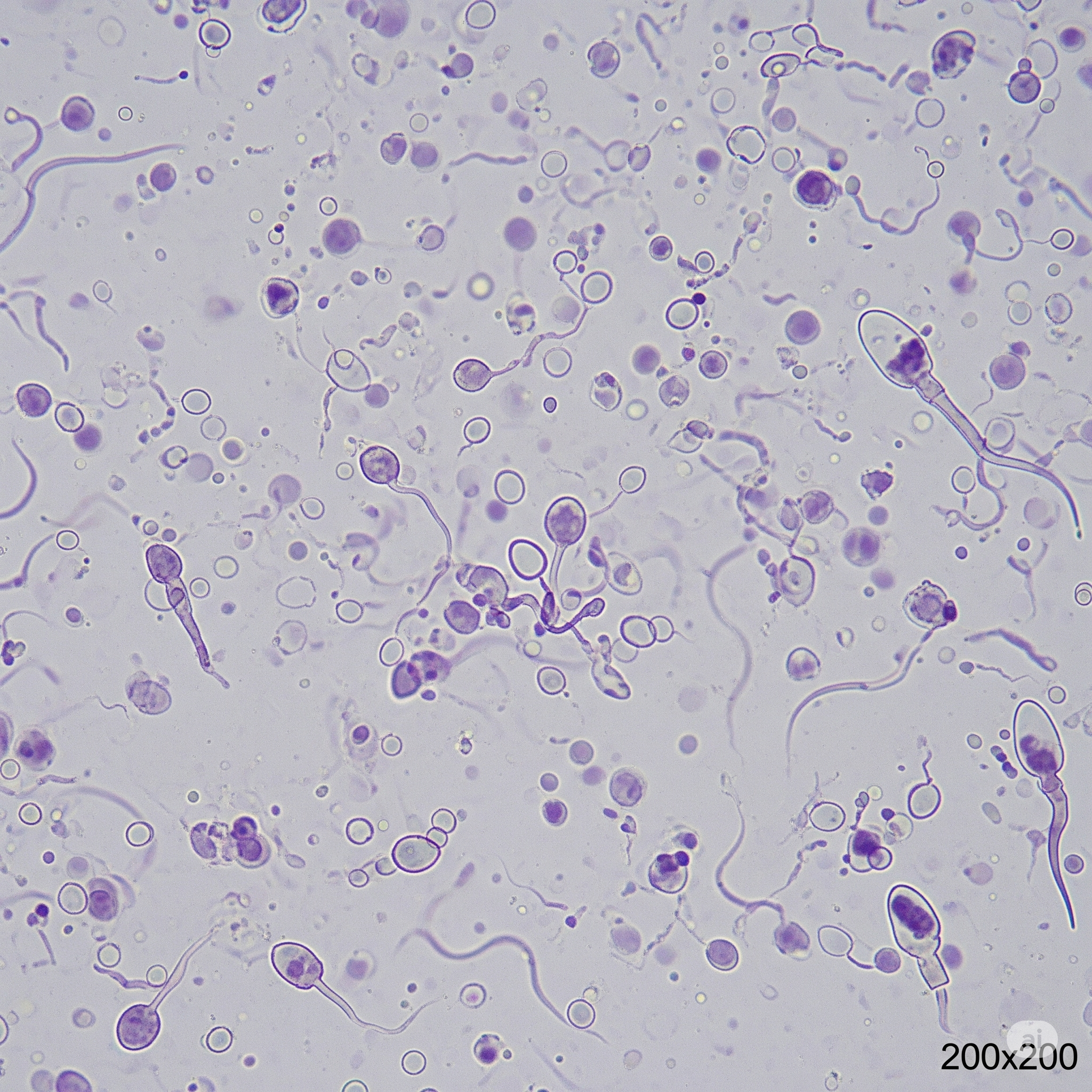
Low Sperm Motility And Morphology Evaluation
Beyond quantity, sperm quality, specifically its ability to move effectively (motility), and its normal shape (morphology), is vital for conception. We conduct detailed evaluations to understand issues like asthenozoospermia (poor motility) or teratozoospermia (abnormal morphology). Our tailored approaches aim to improve sperm function, often utilizing advanced sperm selection techniques for better fertility treatment success.
Azoospermia Evaluation
Azoospermia signifies the complete absence of sperm in the ejaculate. Our comprehensive evaluation includes hormonal tests, genetic screening, and imaging to determine if the condition is obstructive (a blockage) or non-obstructive (impaired production). This critical diagnosis guides treatment decisions, such as the viability of sperm retrieval procedures like TESA or Micro TESE, or considering alternative family-building options.
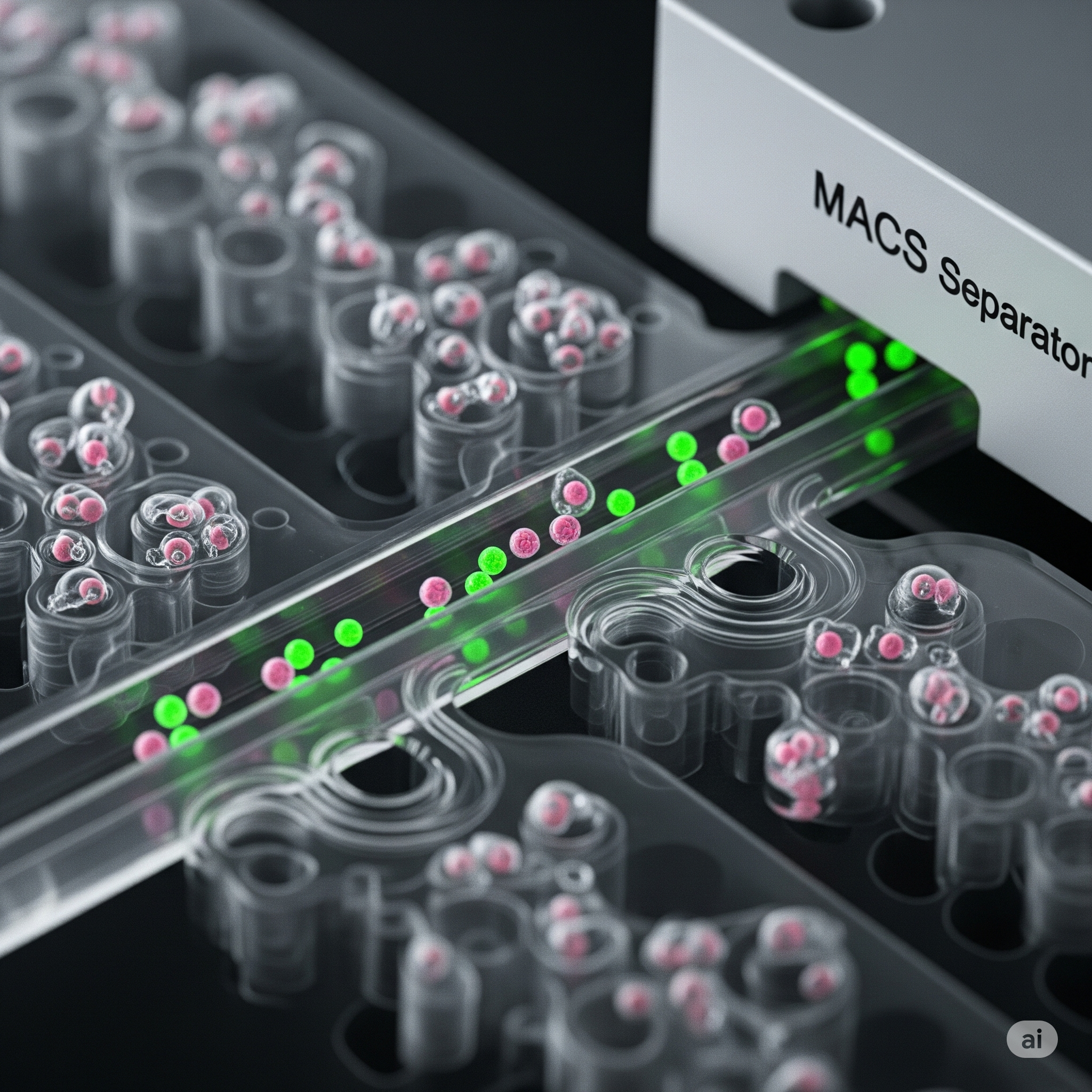
Microfluidics And Magnetic Activated Cell Sorting (MACS)
These advanced techniques are used to precisely select the healthiest and most viable sperm for fertility treatments. Microfluidics gently isolates high-quality sperm by mimicking natural processes, while MACS actively removes damaged or apoptotic sperm using magnetic technology. Employing these methods significantly enhances sperm quality, leading to improved fertilization rates and embryo development in IVF/ICSI cycles.

Testicular Sperm Aspiration (TESA)
TESA is a minimally invasive procedure for sperm retrieval, typically performed under local anesthesia. A fine needle is used to aspirate sperm directly from the testis. This technique is often recommended for men with obstructive azoospermia or those unable to produce sperm through ejaculation, providing viable sperm for IVF with ICSI.
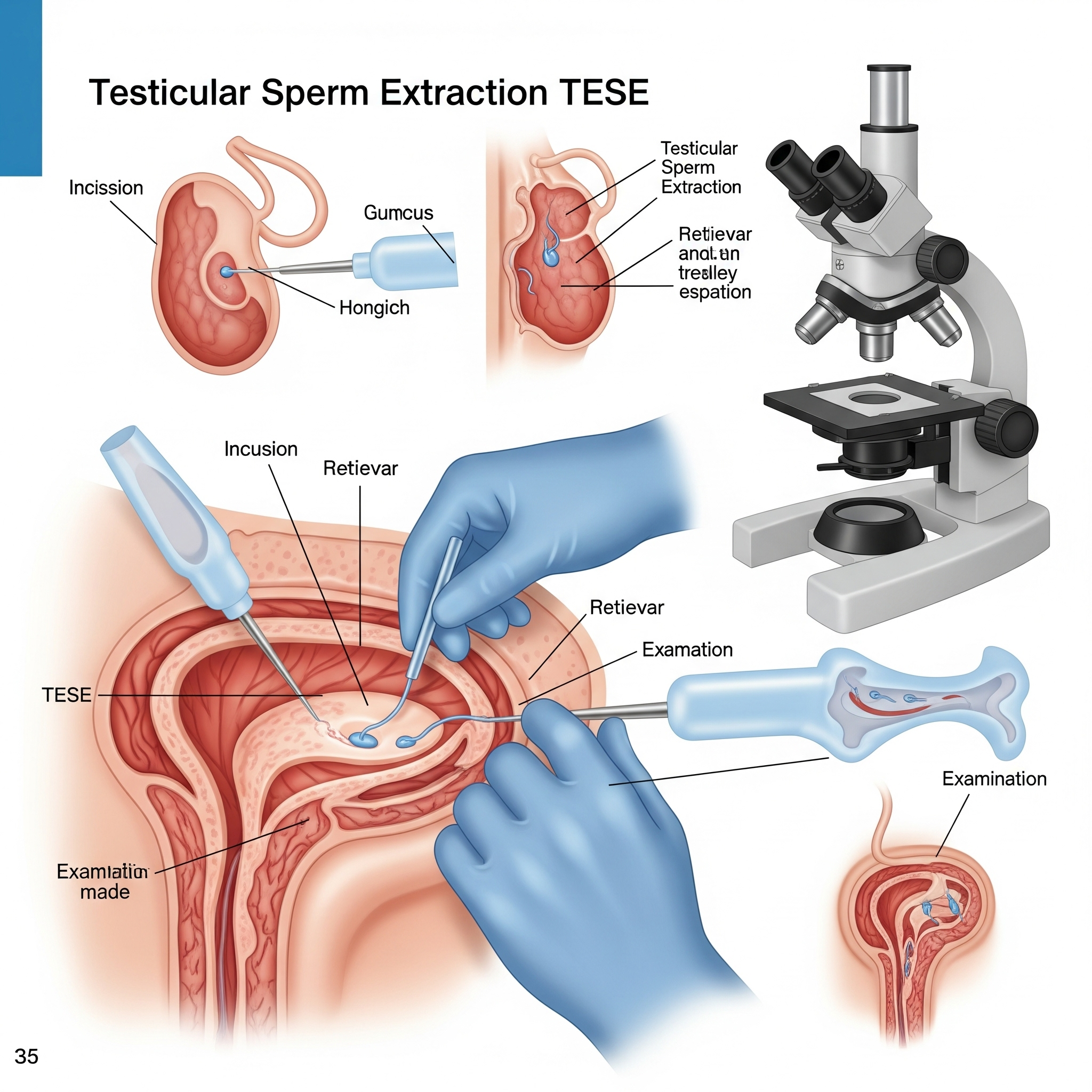
Testicular Sperm Extraction (TESE)
TESE is a surgical procedure to retrieve sperm directly from testicular tissue. It involves taking small biopsies from the testis, which are then processed in the lab to find sperm. This method is often employed for men with non-obstructive azoospermia or when TESA is unsuccessful, offering a viable solution for sperm retrieval for ART.

Micro TESE (Microdissection Testicular Sperm Extraction)
Micro TESE is the most refined sperm retrieval technique, performed using a high-powered operating microscope. This allows the surgeon to meticulously identify and extract seminiferous tubules most likely to contain sperm, even in cases of very low sperm production. This targeted approach maximizes sperm yield while preserving testicular tissue, offering the best chance for sperm retrieval for men with severe non-obstructive azoospermia.